 Scoliosis specific exercises can be done in water, with a kinesiologist, physiotherapist, osteopath or chiropractor.
Scoliosis specific exercises can be done in water, with a kinesiologist, physiotherapist, osteopath or chiropractor.
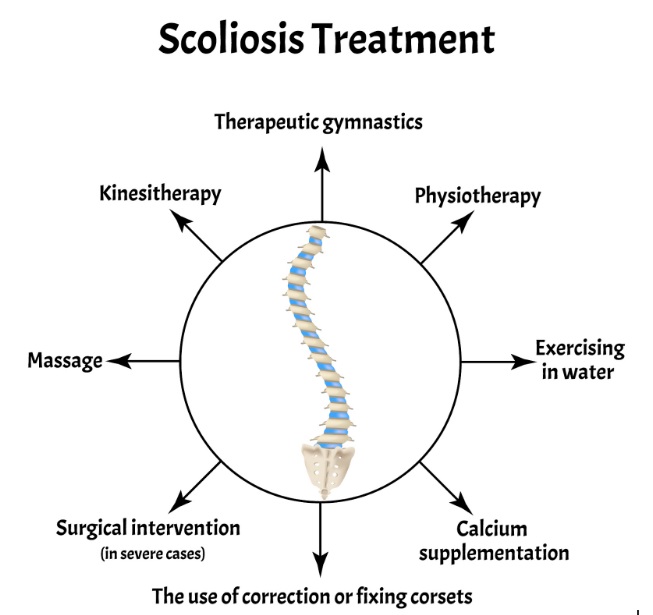 Depending on your age you may also want to consider dietary changes or supplements and more passive therapies like massage and foam rolling. These can help the symptoms of scoliosis which are pain and fatigue and are more common in adults than teens.
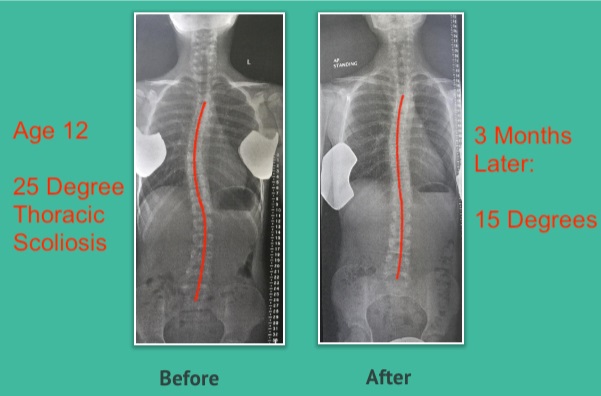
The takeaway here is that your doctor might not even mention other approaches and instead just focus on the angle of the curve and surgery, when specific exercises in adolescence and adulthood can slow down, stop or even reverse the progression of scoliosis.
If you would like to receive my FREE E-book on the 7 Secrets of Scoliosis join the Public Scoliosis Correction Protocol Group here and download it once you join: https://www.facebook.com/groups/351414238781617/
Sources:
Depending on your age you may also want to consider dietary changes or supplements and more passive therapies like massage and foam rolling. These can help the symptoms of scoliosis which are pain and fatigue and are more common in adults than teens.
The takeaway here is that your doctor might not even mention other approaches and instead just focus on the angle of the curve and surgery, when specific exercises in adolescence and adulthood can slow down, stop or even reverse the progression of scoliosis.
If you would like to receive my FREE E-book on the 7 Secrets of Scoliosis join the Public Scoliosis Correction Protocol Group here and download it once you join: https://www.facebook.com/groups/351414238781617/
Sources:

"Oh My Gosh- I am ALREADY feeling relief after a few days! I used to wake up 2-3 times a night with shooting pain that anti inflammatories couldn't touch. Now I have been waking up just because I want to notice what it feels like to lay in bed pain free- THANK YOU!."

"When I first started with your program I was experience a lot of pain. Walking was difficult. I had to stop and catch my breath every few minutes and lean against a wall for support. Now when I walk with my husband we go for over an hour. I never had to sit down and stop...and, hardly any pain!!! 😊😊 I can’t thank you enough."
Frustrated that you aren't recovering fast enough?
Discover how to heal from illness and injury using movement, food and lifestyle.