The shock of discovering scoliosis can be very sudden. Adolescent Idiopathic Scoliosis can feel like it comes on overnight, one day it isn’t there then the next day it is. Or course it doesn’t happen like this but when parents notice it for the first time it seems like it does. If you are like most people, you’ve gone home and googled it. And what do you read?
Most likely you start by reading the definition:
Scoliosis is a condition that causes the spine to curve to the side. It can affect any part of the spine, but the most common regions are the chest area (thoracic scoliosis) and the lower section of the back (lumbar scoliosis). Idiopathic scoliosis has no known cause.
That doesn’t tell you much, so you dig a little further and see something like this from the Mayo Clinic:
“If a scoliosis curve gets worse, the spine will also rotate or twist, in addition to curving side to side. This causes the ribs on one side of the body to stick out farther than on the other side.
Problems with Appearance. — including unlevel shoulders, prominent ribs, uneven hips, and a shift of the waist and trunk to the side
“Complications can involve lung and heart damage, back problems.”
This doesn’t sound good…you don’t know if you or your child’s spine will get worse, get better, or just stay the same.
Your doctor will probably ask for some x-rays. Once they come back, they will measure the change in degrees of your spine from straight to bent, called the Cobb Angle and depending on how severe the curve is, they will give you three options:
- Wait and see what happens to the angle of the curve.
- Bracing
- Surgery
This is pretty typical of modern medicine. They have to draw a line in the sand somewhere, but it doesn’t take into account all the other types of therapy you could try.
Viewing scoliosis simply as an unwanted curvature in the spine means it seems logical that correction is the only solution. For example, if I’m a surgeon trained to fix physical issues through surgery, how would I want to fix a curve? Most likely, I would recommend surgery.
A review of the history of surgery for scoliosis by Carol Hasler in the Journal of Children’s Orthopaedics (1) points out that when the methods used in scoliosis surgery are compared to other orthopedic surgeries such as hip and knee replacements, it is stigmatized by the medical world as ‘a rather archaic way of sacrificing function in young and otherwise healthy individuals.’ However, it’s come a long way from the way Galen and Hippocrates used to treat scoliosis.
In the 1950s, a surgeon named Paul Harrington pioneered a procedure that corrected the side bending of the spine by cutting people along the length of their back and inserting metal rods. It’s been estimated that between 1960 and 1990, about one million people had this surgery. However, it’s no longer used in the original format because it came with numerous problems.
For example, the rods had a tendency to break resulting in more operations. Historically, surgeons didn’t consider the spine as a three-dimensional structure, meaning it moves forward and backward, side to side, and rotates both ways. This resulted in the areas on either end of the rod being overworked, wearing out, and developing arthritis.
Modern Surgical Techniques
During the 1970s and 80s, surgery was developed to work with the three-dimensional nature of the spine by using wires, hooks, screws, and rods. These procedures were refined during the 90s, but still, new surgeries were created due to the shortcomings of the wires, hooks, and rods.
More recently, surgeons offer osteotomies (removal of parts of the bone), vertebral body resection (removal of the vertebra), and most recently, vertebral tethering, in which a surgeon essentially takes some cord and tacks it between two vertebrae on the the long side of the curve. As the person grows, it creates tension and straightens the spine.
Some of these modern surgeries aim to preserve the ability of the spine to function or express movement in young people which is a huge leap forward from the rods.
Before You Commit to Surgery
Don’t get me wrong, I’m not against surgery. But before we commit to a procedure from which there is no turning back at such a young age, we need to ask some pretty deep questions.
- At what point do you need surgery, and what happens if you don’t have it?
Ask your doctor
- At what curve angle is surgery medically necessary due to heart or lung problems?
You’ll be surprised by the answer.
- Ask them what happens if you don’t have surgery?
- Ask them what problems can be caused by the long term loss of motion in the spinal joints after surgery?
If you are not considering surgery then you should look into bracing and exercise.
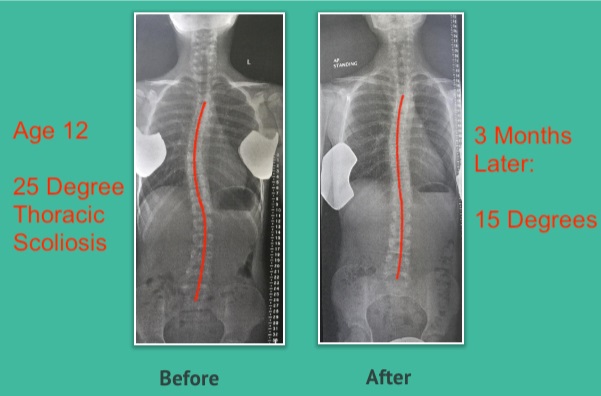
Bracing has been shown to be effective(2) in halting curve progression and exercise can be used in combination with bracing or by itself to slow down, stop or reduce curves. Exercise, in some but not all cases, is also a great way to reverse the curve. For example, Charlotte, at 12 years old, had a curve of 25 degrees, and in just 3 months reduced it by 10 degrees by following the Scoliosis Protocol.
Scoliosis specific exercises can be done in water, with a kinesiologist, physiotherapist, osteopath or chiropractor.
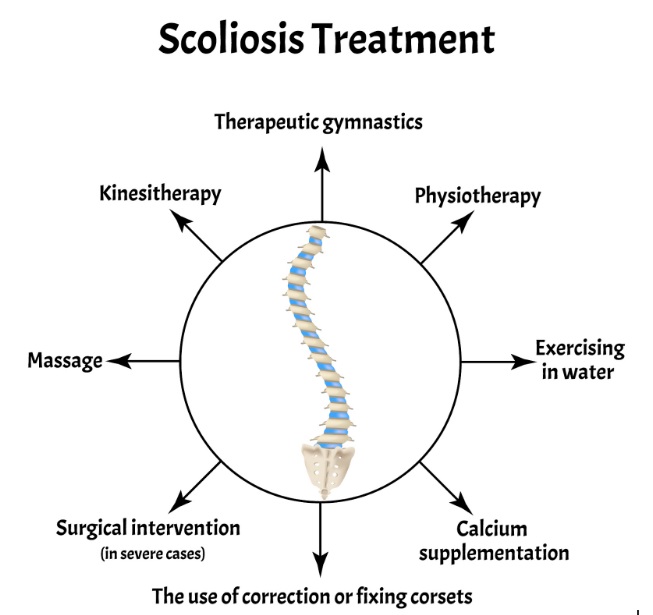
Depending on your age you may also want to consider dietary changes or supplements and more passive therapies like massage and foam rolling. These can help the symptoms of scoliosis which are pain and fatigue and are more common in adults than teens.
The takeaway here is that your doctor might not even mention other approaches and instead just focus on the angle of the curve and surgery, when specific exercises in adolescence and adulthood can slow down, stop or even reverse the progression of scoliosis.
If you would like to receive my FREE E-book on the 7 Secrets of Scoliosis join the Public Scoliosis Correction Protocol Group here and download it once you join: https://www.facebook.com/groups/351414238781617/
Sources:
