Have you ever heard about Metabolic Syndrome?
In simple terms, someone can be diagnosed as having metabolic syndrome if they have 3 or more of the following signs and symptoms:
- Central obesity
- Reduced high-density lipoprotein
- Elevated triglycerides
- Elevated blood pressure
- Elevated fasting blood glucose
Also, people who do have this cluster of signs and symptoms often have chronic diseases such as cardiovascular disease, arthritis, chronic kidney disease, schizophrenia, and several types of cancer. Just in the United States, there are over 3,000,000 new cases alone, with 47 million existing cases.
This “syndrome” is generally considered chronic and lifelong, but what are the criteria for all five risk factors?
Let’s dig down a little and find out a bit more about those markers.
The National Institutes of Health guidelines define metabolic syndrome as having three or more of the following traits, including traits for which you may be taking medication to control:
- Large waist: A waistline that measures at least 35 inches (89 centimeters) for women and 40 inches (102 centimeters) for me.
- High triglyceride level: 150 milligrams per deciliter (mg/dL), or 1.7 millimoles per liter (mmol/L), or higher of this type of fat found in the blood.
- Reduced “good” or HDL cholesterol: Less than 40 mg/dL (1.04 mmol/L) in men or less than 50 mg/dL (1.3 mmol/L) in women of high-density lipoprotein (HDL) cholesterol
- Increased blood pressure: 130/85 millimeters of mercury (mm Hg) or higher.
- Elevated fasting blood sugar: 100 mg/dL (5.6 mmol/L) or higher (pre-diabetic or type 2 diabetic).
So, it’s not really a disease; it’s just a group of conditions that go together. Doctors commonly say there is no definitive cause. However, if we analyze each risk factor, we can start to unpick some of the underlying causes that are ‘pretty well known’.
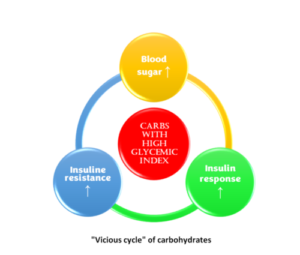
The first fact is that carbohydrates raise blood glucose and are composed of different forms of sugar. They’re quickly absorbed and raise blood sugar. Also, foods that do this can be said to have a high glycemic index. Foods that raise blood sugar also trigger higher insulin responses; if insulin levels are high for a long time, the body develops insulin resistance.
Once you have insulin resistance, the cells don’t respond the same way to sugar, so the glucose rises, and we have a vicious cycle that eventually leads to type 2 diabetes.
When this cycle starts, the second fact comes into the picture. Insulin stimulates the conversion of blood glucose to fat, lipogenesis, and the fat that travels in the blood is called triglycerides; too much of that is the second criterion for diagnosing metabolic syndrome. The third fact is that insulin also slows down the body’s ability to use fat as a fuel source (lipolysis), so insulin promotes the growth of fat and prevents fat burning; hence, it is stored waistlines increase.
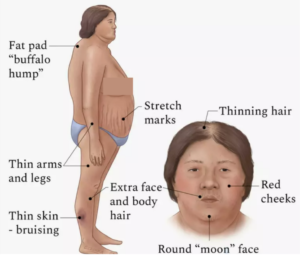
The last fact is that cortisol is a stress hormone that raises blood sugar, leads to insulin resistance, and is very closely associated with belly fat. For example, if a person has too much cortisol, a condition known as Cushing syndrome, they will develop insulin resistance, belly fat, and typical body shapes, as shown in the diagram.
If we correlate the five risk factors with carbs, insulin, and cortisol, we can establish that:
- Cortisol and insulin resistance causes abdominal obesity.
- Raised triglycerides are the result of insulin resistance and high blood sugar.
- High blood pressure is primarily a function of stress and, combined with cortisol, becomes a component of metabolic syndrome by increasing blood pressure.
- Elevated blood glucose results from carbohydrate consumption and high insulin, just like we see in the “vicious cycle” when consuming carbs.
- Reduced HDL and increased LDL are a result of inflammation.
To me, it’s evident that the underlying cause of the metabolic syndrome is insulin, inflammation, and stress. You need to focus on these three things to reverse or prevent getting any of the five risk factors for metabolic syndrome.
How can we treat metabolic syndrome?
Well, let’s look at the standard treatment for metabolic syndrome.
- For abdominal obesity, doctors tell you to lose weight and suggest a “healthy diet” that is high in grains and carbohydrates, rich in fruits, and low-fat dairy or non-fat dairy. However, now you know that all these things have a high glycemic index that will promote insulin resistance.
- They also give you statin drugs for the triglycerides to decrease LDL and consequently help to increase HDL. However, statin drugs interfere with the liver’s cholesterol production, an essential nutrient and one of the building blocks of your brain. They also interfere with the body’s production of coenzyme Q10, the critical enzyme inside the mitochondria that helps the body produce energy. The statins will shut down energy production in the brain, heart, and liver because they’re the most metabolically active. I personally wouldn’t recommend taking statin drugs, but I’m not a medical doctor. So only you and your doctor can make that decision, and if you take any statin drugs, you must supplement with high doses of coenzyme Q10.
- For high blood pressure, doctors can prescribe many drugs, including prescribe beta-blockers, and for type 2 diabetes and high blood sugar, they’ll prescribe insulin or insulin-promoting medication.
You now see why metabolic syndrome is considered chronic and can’t be cured; this problem starts with insulin, insulin resistance, and blood glucose. Yet most treatments promote insulin resistance, and eating a diet high in carbohydrates encourages insulin resistance, and even worse, the same happens with type 2 diabetes. When you take insulin or an insulin-mimicking drug, you trick yourself into becoming more insulin-resistant.
The problem with metabolic syndrome is treating each risk factor (symptom) separately; this happens when we ignore the root cause- and focus strictly on treating symptoms.
So how can you treat the root cause?
The first step is reversing insulin resistance, reducing the intake of foods that stimulate the most insulin and the frequency of meals that promote insulin. This means eating less sugar, fewer carbs, and, for the majority of people with metabolic syndrome, eating fewer calories.
Some options are low-carb keto and intermittent fasting. I’ve tried everything, not because I have metabolic syndrome but because I like to experience any lifestyle modifications firsthand. Personally, I think the easiest intervention most people can do is limit the time window in which they eat. This can lead to weight loss and usually means people don’t snack as much.
Next is reducing inflammation; in general, sugar, gluten in some grains, and insulin cause inflammation. Most people are sensitive or allergic to foods like grains and processed dairy, and in other cases, people are also susceptible to specific foods like strawberries, fish, nuts, or nightshades.
The third, and probably the most impactful thing, is stress because stress contributes to the rise in insulin and inflammation and produces cortisol. Which we now know are the 3 big underlying facts of metabolic syndrome.
I hope people with metabolic syndrome see how a slow, sustainable change in their lifestyle, which focuses on reversing the things that trigger their insulin levels, inflammation, and cortisol level, can lead to better results with metabolic syndrome than just taking drugs for each symptom.
Sources:
https://www.cdc.gov/pcd/issues/2017/16_0287.htm
https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
