Have you ever heard about Metabolic Syndrome?
In simple terms, someone can be diagnosed as having metabolic syndrome if they have 3 or more of the following signs and symptoms:
Also, people who do have this cluster of signs and symptoms often have chronic diseases such as cardiovascular disease, arthritis, chronic kidney disease, schizophrenia, and several types of cancer. Just in the United States, there are over 3,000,000 new cases alone, with 47 million existing cases.
This “syndrome” is generally considered chronic and lifelong, but what are the criteria for all five risk factors?
Let’s dig down a little and find out a bit more about those markers.
The National Institutes of Health guidelines define metabolic syndrome as having three or more of the following traits, including traits for which you may be taking medication to control:
So, it’s not really a disease; it’s just a group of conditions that go together. Doctors commonly say there is no definitive cause. However, if we analyze each risk factor, we can start to unpick some of the underlying causes that are ‘pretty well known’.
The first fact is that carbohydrates raise blood glucose and are composed of different forms of sugar. They’re quickly absorbed and raise blood sugar. Also, foods that do this can be said to have a high glycemic index. Foods that raise blood sugar also trigger higher insulin responses; if insulin levels are high for a long time, the body develops insulin resistance.
Once you have insulin resistance, the cells don’t respond the same way to sugar, so the glucose rises, and we have a vicious cycle that eventually leads to type 2 diabetes.
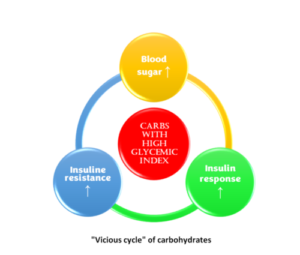
When this cycle starts, the second fact comes into the picture. Insulin stimulates the conversion of blood glucose to fat, lipogenesis, and the fat that travels in the blood is called triglycerides; too much of that is the second criterion for diagnosing metabolic syndrome. The third fact is that insulin also slows down the body’s ability to use fat as a fuel source (lipolysis), so insulin promotes the growth of fat and prevents fat burning; hence, it is stored waistlines increase.
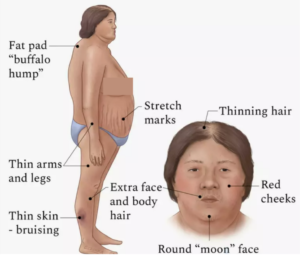
The last fact is that cortisol is a stress hormone that raises blood sugar, leads to insulin resistance, and is very closely associated with belly fat. For example, if a person has too much cortisol, a condition known as Cushing syndrome, they will develop insulin resistance, belly fat, and typical body shapes, as shown in the diagram.
If we correlate the five risk factors with carbs, insulin, and cortisol, we can establish that:
To me, it’s evident that the underlying cause of the metabolic syndrome is insulin, inflammation, and stress. You need to focus on these three things to reverse or prevent getting any of the five risk factors for metabolic syndrome.
How can we treat metabolic syndrome?
Well, let’s look at the standard treatment for metabolic syndrome.
You now see why metabolic syndrome is considered chronic and can’t be cured; this problem starts with insulin, insulin resistance, and blood glucose. Yet most treatments promote insulin resistance, and eating a diet high in carbohydrates encourages insulin resistance, and even worse, the same happens with type 2 diabetes. When you take insulin or an insulin-mimicking drug, you trick yourself into becoming more insulin-resistant.
The problem with metabolic syndrome is treating each risk factor (symptom) separately; this happens when we ignore the root cause- and focus strictly on treating symptoms.
So how can you treat the root cause?
The first step is reversing insulin resistance, reducing the intake of foods that stimulate the most insulin and the frequency of meals that promote insulin. This means eating less sugar, fewer carbs, and, for the majority of people with metabolic syndrome, eating fewer calories.
Some options are low-carb keto and intermittent fasting. I’ve tried everything, not because I have metabolic syndrome but because I like to experience any lifestyle modifications firsthand. Personally, I think the easiest intervention most people can do is limit the time window in which they eat. This can lead to weight loss and usually means people don’t snack as much.
Next is reducing inflammation; in general, sugar, gluten in some grains, and insulin cause inflammation. Most people are sensitive or allergic to foods like grains and processed dairy, and in other cases, people are also susceptible to specific foods like strawberries, fish, nuts, or nightshades.
The third, and probably the most impactful thing, is stress because stress contributes to the rise in insulin and inflammation and produces cortisol. Which we now know are the 3 big underlying facts of metabolic syndrome.
I hope people with metabolic syndrome see how a slow, sustainable change in their lifestyle, which focuses on reversing the things that trigger their insulin levels, inflammation, and cortisol level, can lead to better results with metabolic syndrome than just taking drugs for each symptom.
Sources:
https://www.cdc.gov/pcd/issues/2017/16_0287.htm
https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916

Over the last 10 years Ed has been building a YouTube library to help people manage their own pain or movement limitations and increase performance through exercise. He regularly adds videos so be sure to subscribe and visit regularly


"Oh My Gosh- I am ALREADY feeling relief after a few days! I used to wake up 2-3 times a night with shooting pain that anti inflammatories couldn't touch. Now I have been waking up just because I want to notice what it feels like to lay in bed pain free- THANK YOU!."

"When I first started with your program I was experience a lot of pain. Walking was difficult. I had to stop and catch my breath every few minutes and lean against a wall for support. Now when I walk with my husband we go for over an hour. I never had to sit down and stop...and, hardly any pain!!! 😊😊 I can’t thank you enough."
Frustrated that you aren't recovering fast enough?
Discover how to heal from illness and injury using movement, food and lifestyle.