We all know how pain works right?
We injure an area and the nerves there get irritated and send a signal to the brain which we interpret as pain.
In its most basic form that is true.
Does this apply in all situations?
No, this understanding of pain can’t be applied in all situations. The most extreme example would be the case of phantom limb pain. This is where someone is missing a limb but can still feel itching or pain in it, even though the limb is no longer there. In this case it is obvious that there is no injury in the affected area but the part of the brain that received input from that area is over sensitised and telling the person ‘false’ information.
Don’t people want to know what is causing their pain?
When someone contacts me and says they have had pain for years, most commonly in the back, they frequently tell me that the pain is coming from something like a disc bulge or arthritis and they want surgery to fix it.
Surgery does change structure, and can change things like disc prolapses. However, they are applying the simple understanding of how pain works ie injury to tissue = pain, to their situation. This is often reaffirmed by an x-ray or MRI telling them that there is something structurally wrong….but when we look at the general population we find things like disc bulges and degenerative disc disease are very common in asymptomatic individuals, for example, this study showed the prevalence of disc bulges in asymptomatic populations ranges from 20% in young adults to >75% in patients older than 70 years of age (1).
Why do some people have chronic pain and others don’t.
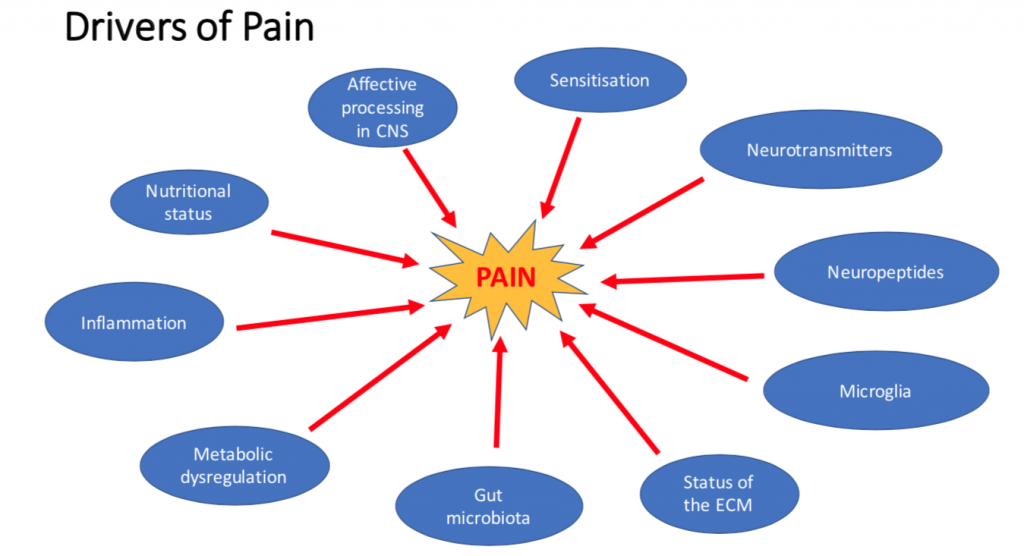
Another way of asking the question is why is this person not able to adapt to their current situation. Science has started to a whole body approach to answer this question. For example, stress is a player in how much pain we feel.
Short term stress to our bodies, minds and spirits can be a good thing. We have evolved to adapt and thrive with it.
The Mayo Clinic describes this natural stress response very well –
“When you encounter a perceived threat — such as a large dog barking at you during your morning walk — your hypothalamus, a tiny region at your brain’s base, sets off an alarm system in your body. Through a combination of nerve and hormonal signals, this system prompts your adrenal glands, located atop your kidneys, to release a surge of hormones, including adrenaline and cortisol.
Adrenaline increases your heart rate, elevates your blood pressure and boosts energy supplies. Cortisol, the primary stress hormone, increases sugars (glucose) in the bloodstream, enhances your brain’s use of glucose and increases the availability of substances that repair tissues.
Cortisol also curbs functions that would be nonessential or detrimental in a fight-or-flight situation. It alters immune system responses and suppresses the digestive system, the reproductive system and growth processes. This complex natural alarm system also communicates with the brain regions that control mood, motivation and fear.” (2)
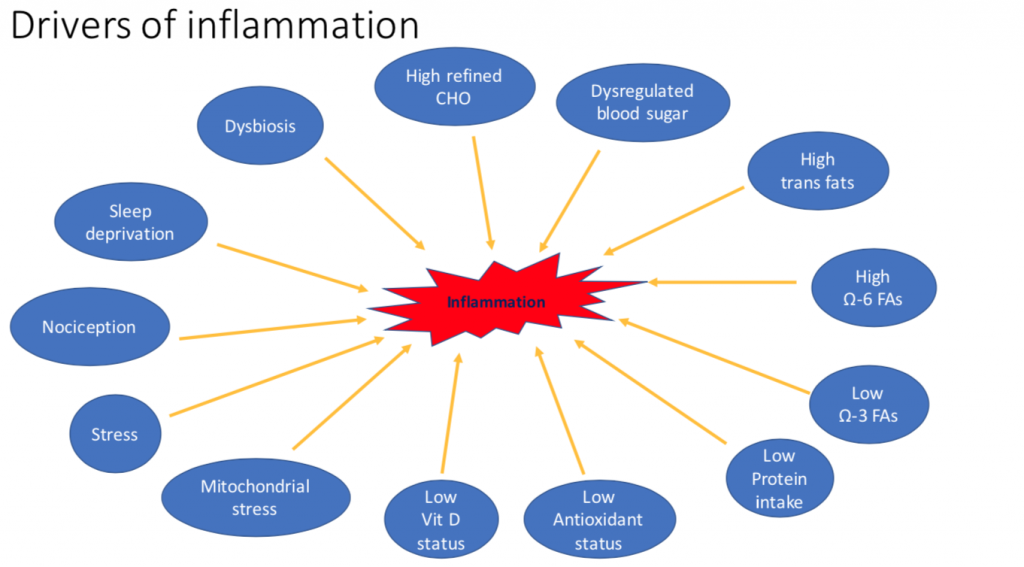
What else does cortisol do?
One of the immune responses cortisol has is to suppress inflammation. The theory for this is that if you are bitten by the dog you don’t want to immediately swell up, you might have to do some running first.
However, our body can’t tell the difference between the acute stress of a dog jumping barking at us and the every day stress of driving in rush hour traffic or commuting on public transport. Therefore, it releases stress hormones every day and over time these can lead to many varied health conditions such as:
Let’s look at some of these in more details.
Sensitisation
You may have heard the term neuroplasticity. This is essentially the way the brain can adapt to new stimulus or recover from injury. This process is also at work in chronic pain.
If the brain has increased ‘nociceptive input’ aka pain, caused by things like injury or inflammation it actually changes how it perceives pain and can become hyper sensitive to signals from that area, which means things like light touch or movement are felt as pain, or you just feel constant pain (4).
Neurotransmitters
These can be seen as either excitatory – meaning they cause inflammation or inhibitory meaning they are anti-inflammatory. Neurotransmitters can be made by the body or are made from amino acids found in the food we eat. Two notable ones, when it comes to pain modulation, are the excitatory amino acid glutamate(5) and the inhibitory one glycine (6). Too much glutamate and pain can be increased. By contrast increasing glycine can help decrease inflammatory diseases. The body produces its own glycine but can also be boosted by eating high-protein foods including meat, fish, eggs, dairy and legumes.
Gut Health
A well functioning digestive system with good gut bacteria can be essential for the maintenance of health, including:
This dysbiosis can happens when we are under stress and not eating healthily.
Interestingly many of the cellular receptors for amino acids are the same in the gut and the central nervous system, this has been described as the gut brain axis that we have heard so much about. Some of these amino acids can promote inflammation of the nerves, so if the gut is not functioning as well as it could it can lead to neural inflammation in the brain and spinal cord.
Here are some other drivers of inflammation:
What can you do about it?
Manage your reaction to stress – meditation type practices are good for this – A reduction in you stress response can also help everything below:
Keep your blood sugar stable – you do this by avoiding binging on sugary foods – more common when you are stressed
Make sure you have sufficient intake of amino acids.
This is especially important for vegetarians and vegans. Most don’t realise that during times of mental or even physical stress their amino acid requirements go up. I’ve treated so many vegans that experience a cascade or injuries, such as tendon problems, muscle tears and joint pain that don’t’ seem to be related to each other. A short change in their diet or supplementation is usually enough to increase their amino acids and break the inflammatory cycles that were happening in their bodies.
Sufficient intake of fats to support anti-inflammatory pathways and a healthy nervous system – the omega oils are important here. These are found in oil fish, grass raised beef and flax seeds – healthy choices.
Foster a healthy microbiome and good gut function. – Lot of leafy green vegetables, fermented foods and if necessary supplementation with pre and probiotics.
Sleep well – no blue light after dark – or wear blue like blocking glasses I like https://www.swanwicksleep.com/products/classic-night-swannies, no T.Vs in the bed room and avoiding caffeine products in the afternoon.
If you follow these practices you will be giving your body the best chance to decrease the drivers of pain and inflammation which will not only improve your general health but also decrease your pain.
2. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress/art-20046037
3. Tsoupras A. et al. Inflammation, not Cholesterol, Is a Cause of Chronic Disease. Nutrients. 2018 May; 10(5): 604.
4. Yang S. and Chang M.C. (2019) Chronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative Affective States. Int. J. Mol. Sci. 2019, 20, 3130
5. Wen ZH et al. (2015) Excitatory amino acid glutamate: role in peripheral nociceptive transduction and inflammation in experimental and clinical osteoarthritis. Osteoarthritis Cartilage. 23(11):2009-16
6. Meerza Abdul Razak et al. (2017) Multifarious Beneficial Effect of Nonessential Amino Acid, Glycine: A Review. Oxid Med Cell Longev: 1716701.
7. Guo R et al. (2019) Pain regulation by gut microbiota: molecular mechanisms and therapeutic potential. Nov. 2019: 123, (5), P637-654

Over the last 10 years Ed has been building a YouTube library to help people manage their own pain or movement limitations and increase performance through exercise. He regularly adds videos so be sure to subscribe and visit regularly


"Oh My Gosh- I am ALREADY feeling relief after a few days! I used to wake up 2-3 times a night with shooting pain that anti inflammatories couldn't touch. Now I have been waking up just because I want to notice what it feels like to lay in bed pain free- THANK YOU!."

"When I first started with your program I was experience a lot of pain. Walking was difficult. I had to stop and catch my breath every few minutes and lean against a wall for support. Now when I walk with my husband we go for over an hour. I never had to sit down and stop...and, hardly any pain!!! 😊😊 I can’t thank you enough."
Frustrated that you aren't recovering fast enough?
Discover how to heal from illness and injury using movement, food and lifestyle.
Leave a Reply